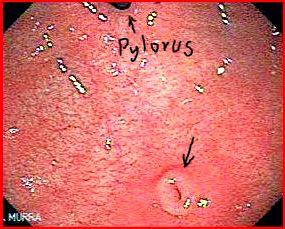
Mr. Wells, a 50 year old school teacher undergo OGD for evaluation of his dyspepsia. It showed:

What is the diagnosis?
Subepithelial mass in the gastric antrum
The term submucosal mass is often used, however it is strictly not correct as the mass may be arising from layers other than submucosa or in fact could be extramural.

Discuss the differential diagnosis of a gastric subepithelial mass?
- GIST (arise from muscle layer)
- Leiomyoma (deep mucosa or muscle layer)
- Carcinoid (arise from deep mucosa or submucosa)
- Lipoma (arise from submucosa)
- Pancreatic rest (arise from deep mucosa or submucosa)
- Duplication cyst (any layer)
Discuss the endoscopic evaluation of a subepithelial mass?
- Intramural mass vs. extrinsic compression: This can be facilitated by changing the patient’s position to see if the location and appearance of the mass changes. Also, a change in appearance of the mass with either air insufflation or deflation may help in determining if the lesion is due to extrinsic compression. However, even when the endoscopist suspects an intramural lesion is present, the mass may arise from outside the gastrointestinal wall in up to 30% of cases.
- Estimate the size: The size of the lesion is important in its management. However, visual inspection may be inaccurate and lead to underestimation of the size of the lesion. Endoscopic assessment of the size can be performed better with an open biopsy forceps (which is 5mm in diameter)
- Mobility and consistency: A mobile mass that is soft and indents when depressed using biopsy forceps (pillow sign) is highly suggestive of a lipoma. A firm, minimally mobile lesion is suggestive of a GIST or leiomyoma.

Discuss your next management steps after endoscopic evaluation?
- If the mass has a pillow sign and is yellow in appearance, it is probably a lipoma and no further evaluation is necessary.
- Subepithelial masses less than 1 cm in diameter are rarely, if ever, of clinical significance. A repeat endoscopy in one year is reasonable for these small masses, and if the mass is unchanged, then further follow-up evaluation may not be required if the patient remains asymptomatic.
- Any subepithelial lesion that appears to be larger than 1 cm on endoscopic examination and does not appear to be a lipoma should be referred for evaluation with EUS.
Would you biopsy?
It is reasonable to obtain mucosal biopsies to exclude epithelial polyps or lesions arising from the deep mucosa. The yield of mucosal biopsies is low, however if the biopsies are positive further investigations may not be warranted. Caution- Biopsy should not be attempted if the subepithelial mass appears to be vascular or cystic.
Discuss the role of EUS in defining subepithelial masses?

- EUS examination differentiates intramural lesions from extrinsic compression.
- EUS can ascertain the exact size, layer of origin, as well as additional morphologic features that can suggest the diagnosis. On EUS the mass can be either homogeneous or heterogeneous and can be hyperechoic, hypoechoic, or anechoic.
- EUS features are used to determine the need for EUS guided FNA or core needle biopsy.
- EUS findings may be sufficiently diagnostic so that further testing, tissue sampling, and follow-up are not required. Intramural anechoic masses without Doppler signals are duplication cysts and are of no clinical significance unless they are causing luminal obstruction. Similarly, densely hyperechoic submucosal masses are always lipomas which also do not have any clinical importance unless they are causing clinical symptoms such as obstruction or bleeding caused by ulceration.
Discuss the role of CT scan or USS in subepithelial masses?
EUS is the investigation of choice for subepithelial masses. However, CT may have a role where EUS is not available:
- CT is most useful in defining the origin and extent of extramural masses.
- Large lipomas or GIST may be visible on CT scan.
Discuss pancreatic rests as a cause of gastric subepithelial mass?
- Pancreatic rests or heterotopic pancreatic tissue is presence of ectopic pancreatic tissue most commonly found in stomach and small intestine. It is a congenital anomaly.
- It typically appears as submucosal mass with a central umbilication in the prepyloric region.
- EUS will show a heterogenous mass arising from the submucosa or deep mucosa with a pancreatic duct remnant. FNA will reveal pancreatic tissue.
- It is a benign and asymptomatic condition. No therapy is warranted.
- Ductal adenocarcinoma, islet-cell tumours, and pancreatitis can arise in heterotopic pancreas tissue, but the rarity of these diagnoses suggests that neither surgical excision nor endoscopic surveillance is warranted.
Discuss the diagnosis in the current case?
EUS revealed a hypoechoic mass arising from the muscle layer. FNA of the lesion was performed. Cytology and immunohistochemistry was diagnostic of a GIST.
Ref:
- Hwang JH et al. The Incidental Upper Gastrointestinal Subepithelial Mass. Gastroenterology 2004;126:301–307
- Carmack SW et al. Management of gastric polyps: a pathology-based guide for gastroenterologists. Nat Rev Gastroenterol Hepatol. 2009;6:331-341
- Link to subepithelial mass section
- Link to GIST section
Image courtesy of www.gastrointestinalatlas.com






