Achalasia cardia (AC)
Discuss achalasia?
- Achalasia means “does not relax” (Greek word)
- Loss of peristalsis in distal (lower two third) oesophagus and failure of LOS relaxation
- Unknown cause
- Results in failure of oesophageal emptying leading to dysphagia
- Achalasia is an uncommon disorder that has an annual incidence of approximately 1 case per 100,000
Discuss the pathology of achalasia?
- Degeneration of inhibitory neurons (ganglion cells) in the myenteric plexus in the oesophagus
- Often surrounded by lymphocytes- so an inflammatory aetiology is suspected
- Selective loss of inhibitory neurons results in unopposed excitation of the LOS by the release of acetylcholine from presynaptic cholinergic nerve terminals in the myenteric plexus
Discuss achalasia like motility disorders (pseudo-achalasia)?
- Manometry can not differentiate between true achalasia and pseudoachalasia
- Careful endoscopy with biopsy is the mainstay of diagnosis
- The different conditions which present as pseudo-achalasia
- Gastric carcinoma
- Chaga’s disease (infection with the protozoan parasite Trypanosoma cruzi can result in a loss of intramural ganglion cells leading to aperistalsis and incomplete LES relaxation)
- Eosinophilic gastroenteritis
- Sarcoidosis
- Amyloidosis
- Chronic idiopathic intestinal pseudo-obstruction
Discuss the clinical features of achalasia?
- Men and women are affected with equal frequency.
- The disease can occur at virtually any age, but onset before adolescence is unusual.
- Dysphagia for solids and liquids is the primary clinical feature of achalasia
- Dysphagia for liquids is most characteristic of achalasia and strongly suggests the diagnosis.
- Difficulty belching is present in approximately 85 percent of patients. Few describe this symptom spontaneously.
- Weight loss, regurgitation, chest pain, and heartburn can occur. Regurgitation of material at night may result in aspiration.
- GORD symptoms occurs with surprising frequency in achalasia – probably by direct inflammation of the mucosa by the food, pills, or lactate production by bacterial fermentation of retained carbohydrate.
Discuss the risk of cancer in achalasia?
- Substantially increased risk of squamous cell oesophageal cancer approx 15years after diagnosis.
- Insufficient data to support routine endoscopic surveillance for patients with achalasia
Discuss the investigations for achalasia?
CXR
- Occasionally widening of the mediastinum due to the dilated oesophagus
- Absence of the normal gastric air bubble
Barium Swallow
- Dilated oesophagus that terminates in a beak-like narrowing caused by the persistently contracted LOS
- The diagnostic accuracy of barium swallow for achalasia is approximately 95 percent
Manometry
- High pressure in the LOS at rest ( usually above 45mm Hg normal being 10mm)
- Failure of the LOS to relax after swallowing
- An absence of useful (peristaltic) contractions in the lower oesophagus. The last two features are the most important and are required to make the diagnosis.
Endoscopy
- Normal in 40% of patient. There may be residual food in a dilated oesophagus
- Evidence of local inflammation may be there.
- Might find resistance while passing the GOJ
- Always look at the fundus and if suspicious take biopsy- to exclude pseudo-achalasia
Discuss the management of achalasia?
Treatment options
- Graded pneumatic dilatation (PD)
- Intramuscular Botulinum toxin injection (Botox)
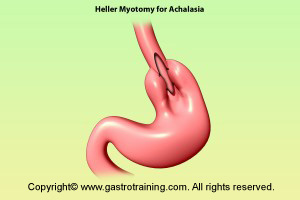
- Hellar’s modified myotomy with or without fundoplication ( open or laparoscopic)
Treatment flowchart
- Approach to patients with achalasia takes into account many factors including age, patient expectations and preferences, and individual risk factors.
- For younger patients at low surgical risk Laparoscopic myotomy is the first choice
- Patients who are reluctant to undergo surgery are offered pneumatic dilation.
- Use of Botox is limited to elderly patients who present a prohibitive risk for surgery or PD.
Graded Pneumatic Dilatation
- There is 50% chance that patients will require another dilatation within 5 years. However, some people have remained symptom-free for as long as 25 years.
- There is a 2-6% risk of perforation usually in the first dilatation session. Most perforations are small and some heal on their own with antibiotics and intravenous feeding.
Botox
- Botulinum neurotoxin type A -reduce the LOS pressure by selectively blocking the release of acetylcholine from presynaptic cholinergic nerve terminals in the myenteric plexus
- 100u of Botox is normally injected in four quadrant in the GOJ in the muscle layer- approximately 1 cm above the Z line using a standard sclerotherapy needle
- Potential complications- very safe. Occasional reports of pneumothorax and fistula formation.
- Current use is limited to elderly or infirm patient in which PD or surgery pose unacceptable risks. It may also be useful as a diagnostic test in patients in whom the diagnosis is uncertain based upon manometric criteria
- Almost all patients treated with Botox relapse after a single injection, usually in the first year or so.
Surgery
- Laparoscopic Heller myotomy is considered to be the primary treatment for achalasia by many because of excellent results, a short hospital stay (1-2 days) and a faster recovery time (regular activities in 2 weeks). Heller’s myotomy often leads to postoperative GORD and hence most surgeons add partial fundoplication to laparoscopic Heller’s myotomy.
- Surgical myotomy results in sustained remission rates of approximately 70 to 85 percent at 10 years, and 65 percent at 20 years.
- The overall complication rate of laparoscopic myotomy is around 6 percent, while mortality rate of approximately 0.1 percent is similar to that reported for pneumatic dilation
Discuss surgery after prior Botox or PD?
- In a prospective series of 154 patients who had undergone previous botulinum toxin injection and/or PD (100 dilation only, 33 Botox only, 21 both), there were significantly more intraoperative complications (mainly oesophageal perforation) compared with patients who did not undergo preoperative therapy (10 versus 4 percent).
- In addition, postoperative complications (mainly dysphagia) were more common in the group that had preoperative therapy (10 versus 5 percent).
- After an average follow-up of 21 months, there was a higher rate of failure in the endoscopically-treated group as compared with treatment of naïve patients (20 versus 11 percent).
- Smith CD et al: Ann Surg. 2006 May;243(5):579-86
- So treatment of choice in fit young patient is surgery rather than PD or Botox.
Technique of balloon dilatation
- The patient is advised to fast for at least 12 hours prior to the procedure +/-liquid diet for one or two days preceding the dilation in patients where regurgitation of old food is a predominant symptom.
- A 30 mm balloon is used for a first dilatation. Subsequent dilatation may involve larger balloon- 35 and 40cm. These are quite big sized balloon compared to standard stricture dilatation balloon the idea being to rupture the muscle fibres.
- Inflate the balloon and check for any leaks.
- A thorough endoscopic examination is performed, with particular attention given to the cardia, where malignancy can simulate achalasia (pseudoachalasia).
- A guidewire is passed through the biopsy channel of the endoscope into the stomach and the scope is withdrawn to the GOJ.
- Note the distance between the incisors and the GOJ should be noted along the length of the scope.
- The endoscope is then removed (taking care to maintain the position of the guidewire in the stomach- push/pull technique).
- As an aid in initial placement, a marker (such as a paper tape/ tippex) can be placed on the shaft of the dilating catheter to correspond to the previously noted distance from the incisors to the GOJ.
- This distance should be measured from the middle of the balloon on the dilating catheter.
- The balloon and tip of the shaft is lubricated and passed over the previously placed guide wire until the marker is in place at the incisors.
- Using fluoroscopy, the balloon is then gradually inflated with air, noting the position of the developing waist.
- Small adjustments usually have to be made in the position (deflating the balloon each time) to ensure that the waist occupies the centre of the balloon- balloon will slip downwards if you are too down and then you will have to exert a pull upwards and vice versa
- After a satisfactory position is obtained, the balloon is fully inflated (usually requiring about 120 mL of air).
- About 7 to 15 PSI of pressure is required for waist obliteration. The balloon is kept inflated for 60 seconds, during which patients may be intensely uncomfortable- give a dose of opiate 2mts before the dilatation
- After the 60 seconds are over, the balloon is rapidly deflated.
- Thereafter, perform another full inflation for 60 seconds and again note the pressure required to obliterate the waist. This is usually at least 3 PSI less than the initial pressure
- The patient is observed for the next five to six hours during which serious complications, such as perforation would be obvious and some do routine post procedure CXR before allowing to eat.







