Jejunum and ileum
Discuss the anatomy of jejunum and ileum?
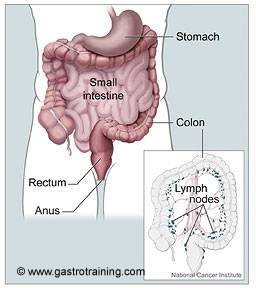
Jejunum begins at the DJ flexure. Together the jejunum and ileum are about 5-8 metres long; jejunum constitutes about two-fifths and ileum comprises the remainder. There is no clear line of demarcation between jejunum and ileum.
Jejunum is thicker, more vascular and redder than ileum. The mucosal folds (valvulae conniventes) are well developed in jejunum, whereas they are small in the proximal part of ileum and absent in its distal part.
The jejunum and ileum is suspended by a mesentery from the posterior abdominal wall. The blood vessels, lymphatics and nerves run between the two layers of the mesentery.
Discuss the blood supply of jejunum and ileum?
Jejunal and ileal branches from the superior mesenteric artery. The arteries unite to form arches from which vasa recta raise and supply the intestine.
Discuss the lymphatic drainage of the jejunum and ileum?
The lymph drain into the mesenteric nodes which then drain in the superior mesenteric lymph nodes. The mesenteric nodes are situated in three positions:
- Close to the wall of the intestine
- Amongst the arterial arches
- Along the superior mesenteric artery
What is Meckel’s diverticulum?
It is a remnant of the vitello-intestinal duct that occasionally persists in the adult as an ileal (Meckel’s) diverticulum, which is situated near the ileocolic junction. It may contain gastric or pancreatic tissue, and inflammation of the diverticulum may simulate acute appendicitis.
Discuss the histology?
Mucosa
Epithelium
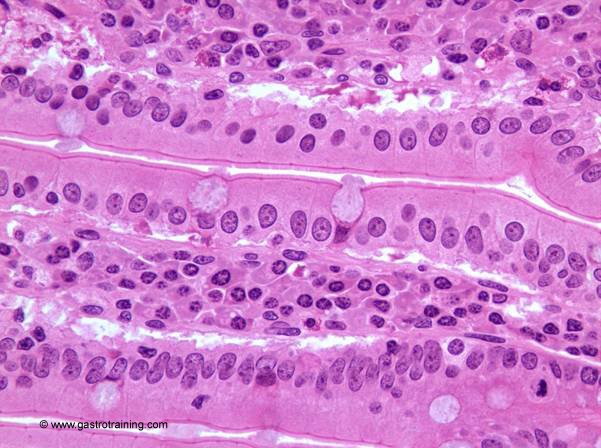
Small intestinal mucosa is specially adapted to increase the luminal surface area to facilitate absorption. The mucosa and submucosa form crescent shaped folds called plicae circulars. These extend around one-half to two-thirds of the circumference of the lumen of the small intestine. Plicae circulars are absent from proximal parts of the duodenum and the distal part of the ileum. The entire intestinal mucosa forms intestinal villi (about one mm long). The surface of the villi is formed by a simple columnar epithelium. Each absorptive cell or enterocyte of the epithelium forms numerous microvilli. Plicae circulars, villi and microvilli tremendously increase the absorptive surface area
Crypts of Lieberkuhn- these are simple tubular glands opening between the intestinal villi. They extend through the lamina propria down to the muscularis mucosae. Function of the crypts of Lieberkuhn:
- Paneth cells located at the bottom of the crypts release antibacterial substances (e.g. lysozyme) to control infections.
- Undifferentiated cells close to the bottom of the crypts regenerate the epithelium.
- Secretion of intestinal juice (about 2 litres/day).
In addition to enterocytes, the epithelium is composed of mucus-secreting goblet cells and endocrine cells. Endocrine cells secrete gastrin, somatostatin, cholecystokinin and secretin. Cholecystokinin stimulates pancreatic digestive juice secretion and the contraction of the gall bladder. Secretin also stimulates the pancreas to release pancreatic juice rich in bicarbonate ions. Secretin also amplifies the effects of cholecystokinin.
Lamina propria- is cell rich. Lymphocytes form solitary lymphoid nodules in the lamina propria. These lymphoid nodules may form large aggregation called Peyer’s patches in the ileum.
Muscularis mucosae- extend into the intestinal villi, where the smooth muscle cells form a longitudinal bundle in the centre of the villi.
Submucosa
The submucosa contains glands (Brunner’s glands) only in the duodenum.
Muscle layer
Serosa
Pic 1 Anatomy
Pic 2 Jejunal mucosa
Pic 3 Jejunal Goblet cell







