Sengstaken-Blakemore tube insertion
The module covers:
- What is Sengstaken-Blakemore tube
- When to use SB tube
- What do you need before you start
- How to actually insert it
- How to maintain traction
- Aftercare and removal
What is Sengstaken-Blakemore tube
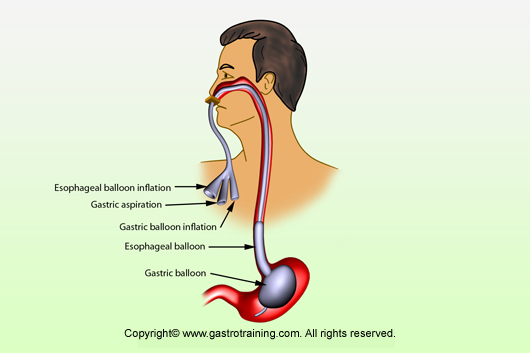
Sengstaken-Blakemore tube is a 3 lumen tube- one lumen to inflate gastric balloon, a second lumen to inflate oesophageal balloon and a third lumen to aspirate gastric contents. There is no oesophageal suction port. This causes saliva to pool in the oesophagus and thus put patients at risk of aspiration.
Commonly Minnesota tube is referred to as Sengstaken-Blakemore tube


Picture1:Minnesota tube or Modified Sengstaken-Blakemore tube
Minnesota tube- or modified Sengstaken-Blakemore tube is a four lumen tube with an additional lumen to aspirate oesophageal lumen to prevent aspiration from swallowed saliva and blood from the oesophageal varix
Linton-Nachlas tube: Single 600ml gastric balloon only
When to use SB tube
It is used in life threatening upper GI bleed from ruptured oesophageal/gastric varices when traditional treatment with band ligation or glue injection has failed or are not available
This is only temporary method to buy time for more definitive procedures to stop the bleeding.
What do you need before you start
- The SB tube is normally kept in freezer- it helps insertion by improved stiffness
- Keep ready two bladder wash syringes for suctioning the oesophageal and gastric lumen, another bladder wash syringe for inflating the gastric balloon
- Stout metal artery forceps for clamping the balloon ports
- If oesophageal balloon needs to be inflated in addition to the gastric balloon- You will need:
- A 50cc Luer Lock syringe
- An adaptor whose conical end will fit into the oesophageal port and the Luer lock end will fit into the sphygmomanometer ( the adaptor is available in the chest drain kit )
- A three way valve
- A sphygmomanometer with detachable arm cuff– to remove the BP cuff and fit the Luer lock end of the chest drain adaptor to fit there
How to actually insert it
- Debate regarding optimal place for the procedure: Resus vs. theatre: anaesthetist prefers theatre
- Patient in normal endoscopy position
- Airway protection- in general, patients who require balloon tamponade to control variceal bleeding should also be intubated. However airway protection is particularly important in
- Encephalopathy
- If Sao2<90%
- Aspiration pneumonia
- Check the balloons by inflating air and checking for any leak
- Smear plenty of KY gel and pass the tube through the mouth like an NG tube- It is kept in the freeze in theatres and Endoscopy unit-to increase the stiffness. Sometimes because of the curled position in which it is stored makes it very difficult to insert like NG tube and a laryngoscope and Magill’s forceps may be needed to guide it past crico-pharyngeus.
- Once it has gone up to 45cm mark it’s tip is expected to lie in the gastric lumen- confirm by aspirating stomach content and checking pH – position to be checked later by portable CXR.
- Once you are sure the tip is in the stomach, inflate the gastric balloon by inflating it with 200ml of air (and put two artery forceps as clamp and also insert the pegs supplied with the tube) and gently tugging it. Some prefer to put contrast mixed water rather than air.
- It should slide for some length and then halt as it abuts against the GOJ –then push additional 50-100ml of air and pull the tube out to exert the pressure on the GOJ.
- For majority of patients this is enough to stop the variceal haemorrhage. However, oesophageal balloon will need to be inflated, if the bleeding continues in spite of the gastric balloon inflation.
- Clamp the tube in between air refills
- Finally fix the tube and keep a record of the distance of the tip from the incisor teeth- normally around 30-35cm mark
- Initial success to control bleeding depends on
- Operator experience
- Concomitant therapy ( Terlipressin and antibiotics )
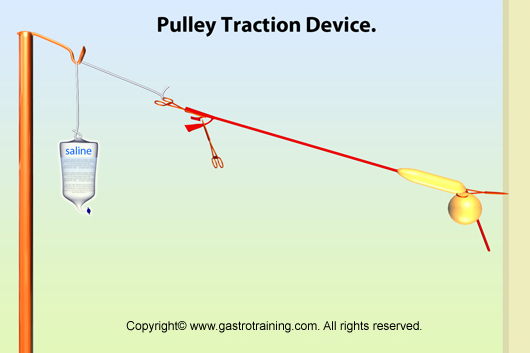
- To maintain the pressure on GOJ- you will have to fix the tube with continued traction. We have noticed a variety of practices
- To hang a bag of 500ml of saline by tying it to the loop of the clamp attached to the tube – the advantage of this technique is
- Bag of saline is universal as opposed to a tennis ball- but units who use tennis ball normally store one ball with the tube
- No pressure on the cheeks/lips unlike the tennis ball
- The traction is measured ( 0.5 kg weight ) unlike unquantifiable traction strength which might vary from person to person
- See the picture of how to do it below.
- To hang a bag of 500ml of saline by tying it to the loop of the clamp attached to the tube – the advantage of this technique is
- If oesophageal balloon is inflated pressure should be accurately measured with a sphygmomanometer.
- Inflate it to 25-40mm Hg. Normal portal pressure is <10 mm Hg; maximal pressure in portal hypertensive patients is never >30 mm Hg, therefore a pressure of 40 mm Hg is sufficient and remember the less the better.

Picture2: Checking for leak
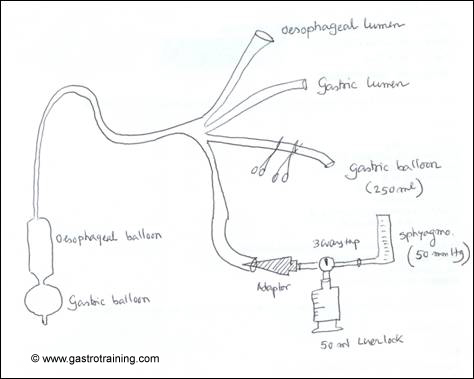
Picture3: The setting up of Modified Sengstaken-Blakemore tube
How to maintain traction
b. Pull the tube and fix it on the side of the cheeks with elastoplasts under tension- not very reliable as elastoplast may become loose and also the traction force will vary among individuals. However this is the most common practice.
c. Another method is to pull the tube and fix it on the side of the cheeks by passing it through a split tennis ball
Aftercare and removal:
- Migration of gastric balloon in oesophagus can cause compression of trachea and respiratory distress. Keep a pair of scissors ready at the bedside in case of emergency – to cut the gastric balloon port to let the air escape
- Instruction to suction both oesophageal and gastric lumen at intervals of 10 minutes increasing to 30 minutes and after stabilization hourly
- Frequent oropharyngeal suction
- Don’t forget antibiotic prophylaxis and continued terlipressin for at least 48hrs
- Pressure in the oesophageal balloon to be relieved for 10minutes every 2hours to prevent pressure necrosis
- Repeat endoscopy at 24 hours.
- The Sengstaken tube should be removed in the endoscopy room
- First deflate the oesophageal balloon, then take off the traction and finally remove the tube
- Chance of rebleeding when balloon is deflated is up to 50%
- On second endoscopy it should be much easier to band or inject glue as bleeding hopefully would be under control, failing which patient should be referred for urgent TIPSS.
- Serious complication can occur up to 15-20%
- Oesophageal ulceration
- Aspiration pneumonia
Here is the link for Sengstaken tube insertion video:
No video found so far. One good link is http://emedicine.medscape.com/article/81020-media
Acknowledgement/Bibliography:
- Helmy A et al. Review article: current endoscopic therapeutic options in the management of variceal bleeding. Aliment Pharmacol Ther. 2001 May;15(5):575-94.
- Seet E et al. The Sengstaken-Blakemore tube: uses and abuses. Singapore Med J. 2008 Aug;49(8):195-7.
- Han HY et al. Simple method for inflating and measuring oesophageal balloon pressure of Sengstaken-Blakemore tube. Intern Med J. 2006 Oct;36(10):684-5.
- Kashiwagi H et al. Technque for positioning the Sengstaken-Blakemore tube as comfortably as possible. Surg Gynaecol Obstet 1991; 172





