Surgery for Peptic Ulcer Disease
Discuss the role of surgery in the management of peptic ulcer disease?
Current indications for ulcer surgery include:
- Failure of medical management of an ulcer complication.
- Suspicion of malignancy (usually in a gastric ulcer)- Even if biopsies are benign, a gastric ulcer that has failed to heal after 12 weeks of medical therapy is usually considered an indication for operation.
More controversial and infrequent indications include:
- Intolerance or noncompliance with a medical regimen.
- Patients who are at high risk for ulcer complications, such as transplant recipients, and those who are steroid or NSAID-dependent.
Discuss the operations for duodenal ulcer?
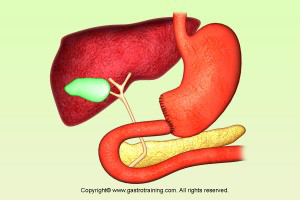
Acid secretion by the parietal cells is normally stimulated by acetylcholine from the vagus nerve and gastrin release from the antrum. The surgical approaches thus attempt to reduce the acid secretion by:
a. Sectioning the vagus (vagotomy) – this eliminates direct cholinergic stimulation to acid secretion.
Three different types of vagotomy are performed: truncal, selective, and highly selective (also referred to as parietal cell or proximal gastric vagotomy).
Truncal —it markedly alters gastric motility. It impairs both the receptive relaxation of the stomach and gastric emptying. Gastric emptying of liquids is speeded with the loss of relaxation, whereas solid evacuation is slowed significantly, leading to gastric stasis. Thus some form of gastric emptying procedure (pyloroplasty or gastroenterostomy) must be performed.
Selective — Truncal vagotomy sacrifices innervation to the pancreas, small intestine, proximal colon, and hepatobiliary tree. Selective vagotomy spares the hepatic and celiac divisions of the vagal trunks. The technique was introduced with the hope that limiting vagotomy to the stomach will result in milder postoperative metabolic and digestive sequelae. A drainage procedure is still required since the antrum is denervated. Prospective studies have failed to show substantial benefit over truncal vagotomy, and selective vagotomy has fallen out of favor.
Highly selective — The rationale for highly selective vagotomy is to eliminate the vagal stimulation to the acid-secreting portion of the stomach without interrupting motor innervation to the antrum and pylorus.
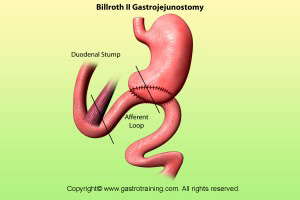
Truncal vagotomy with antrectomy — Truncal vagotomy with antrectomy has been among the most commonly performed procedures for duodenal ulcer disease. The simultaneous effects of vagotomy and antrectomy remove both the cholinergic and gastrin stimulus to acid secretion. After partial gastrectomy, gastrointestinal continuity must be restored by some form of reconstruction. The remnant is anastomosed either to the duodenum (Billroth I) or, after closing the duodenal stump, to the jejunum distal to the ligament of Treitz (Billroth II). The latter has both an afferent limb from the duodenum and an efferent limb extending distally.
Discuss the operations for gastric ulcer?
Since the gastric ulcer may harbor malignancy, the traditional surgical approach has been excision. Operative treatment of gastric ulcer depends on the location of the ulcer:
- Antral ulcer- Distal gastrectomy with Billroth I or II reconstruction is recommended for most patients.
- Prepyloric ulcer- Treatment is similar to duodenal ulcer, with vagotomy and antrectomy the preferred approach.
- Proximal gastric ulcer- subtotal gastric resection (including the ulcer bed) is considered optimal. Alternatives include a distal gastrectomy which is extended along the lesser curvature to include the ulcer.
Discuss the sequelae of surgery?
Postgastrectomy syndromes- are caused either by vagotomy or resection or both. Almost all patients develop a change in their digestive habits postoperatively, however most are able to adapt with time. A significant minority are significantly debilitated by these syndromes.
Postvagotomy diarrhea — it may be related to the rapid passage of unconjugated bile salts from the denervated biliary tree into the colon, where they stimulate secretion. Most cases are self limiting; oral cholestyramine, which binds bile salts, can be effective in persistent cases.
Dumping – it occurs after gastrectomy or vagotomy and drainage. Affected patients have postprandial nausea, vomiting, diarrhoea, and cramps, with vasomotor symptoms such as diaphoresis, palpitations, and flushing. The likely cause is due to the rapid emptying of hyperosmolar chyme into the small bowel. This causes net fluid retention due to the osmotic gradient and release of vasoactive hormones like serotonin and VIP.
Less often, patients complain of the same constellation of symptoms hours after eating, so-called late dumping. This phenomenon is thought to be secondary to hypoglycemia from a postprandial insulin peak.
Most patients with dumping can be treated successfully with dietary changes (frequent small meals that are high in protein and fat and low in carbohydrates for early dumping; increased carbohydrate consumption for late dumping). Octreotide or an analogue may help in severe cases.
Surgical therapy to delay gastric emptying (as with the conversion of a vagotomy and pyloroplasty to an antrectomy with Roux-en-Y reconstruction) may be needed, if the symptoms are intractable.
Alkaline reflux gastritis — Reflux of bile into the stomach is common after operations that eliminate the pyloric sphincter. This usually causes no symptom; however, some patients develop persistent burning epigastric pain and chronic nausea that is aggravated by meals. There is no effective treatment.
Early satiety — early satiety may be due to gastric stasis or resection. Symptoms consist of epigastric fullness with meals, often followed by emesis. Small and frequent meals help besides prokinetic agents. There is anecdotal evidence that gastric pacing may prove useful.
Afferent and efferent loop syndromes — these develop after Billroth II reconstruction or gastroenterostomy. They are related to mechanical obstruction of the limbs by kinking, anastomotic narrowing, or adhesions. Afferent loop syndrome is associated with postprandial epigastric pain and nonbilious vomiting that is then relieved by projectile bilious vomiting. The detection of distended afferent loop on CT is diagnostic. Conversion to a Roux-en-Y anastomosis is necessary to treat this problem. Efferent loop syndrome is associated with epigastric pain, distension, and bilious vomiting; operation is the treatment of choice.
Gastric cancer risk — Patients who have undergone gastric resection for benign gastric or duodenal ulcer disease may be at increased risk for development of gastric cancer, 15-20 years after the initial surgery. The risk in various series has ranged from less than 1 percent to as high as 9 percent, although an increased risk has not been uniformly reported.
Billroth I