Obscure gastrointestinal bleeding (OGIB)
Define OGIB?
OGIB is defined as bleeding of unknown origin that persists or recurs after an initial negative endoscopic evaluation including colonoscopy and/or OGD.
OGIB can be classified as either:
- Occult OGIB, which is manifested by recurrent iron deficiency anaemia and/or recurrent positive faecal occult blood test results; or
- Overt OGIB, which is manifested as melaena or haematochezia.
Discuss the aetiology of OGIB?
- The cause of OGIB is usually a lesion located in the small bowel, but also includes lesions that were overlooked during conventional endoscopy, either because of intermittent bleeding or truly missed lesions.
- The most common lesions giving rise to OGIB in the small bowel are angiodysplasia and tumours.
- However, the aetiology of small intestinal bleeding is dependent on the age of the patient. Younger patients are likely to have small intestinal tumours (leiomyomas, carcinoids, lymphomas and adenocarinomas), Meckel’s diverticulum, Dieulafoy’s lesion, and Crohn’s disease, while older patients (older than 40 years) are prone to bleeding from vascular lesions, which comprise up to 40% of all causes, and NSAID induced small bowel disease. Less common aetiologies of bleeding that originate in the C-loop of duodenum include hemobilia, hemosuccus pancreaticus, and aortoenteric fistula.
- One should be aggressive in the investigation of the aetiology of bleeding in younger patients because small bowel tumours are the most common cause of obscure bleeding in patients younger than 50 years.
Who to investigate?
The cause of GI bleeding in a large proportion of patients with an initially normal endoscopy (upper and lower) resolves spontaneously. Patients with persistent Iron Deficiency Anaemia/FOBT positivity or overt blood loss require further investigation.
How to investigate?
Repeat OGD and/or colonoscopy
Repeat colonoscopy and OGD should be considered prior to evaluation of the small bowel, because lesions missed on initial exam are not uncommon. Commonly overlooked lesions in the upper GI tract include Cameron’s erosions in large hiatus hernias, fundic varices, peptic ulcer disease, angioectasias, Dieulafoy’s lesion, and gastric antral vascular ectasia. Lesions missed during colonoscopy include angioectasias and neoplasms. The diagnostic yield of repeat OGD is sufficient to recommend a second-look endoscopy. Yield of repeat colonoscopy is low (6%).
Wireless capsule endoscopy
Both BSG and AGA recommends it as the third investigation for OGIB. It is non invasive and allows examination of most of the small bowel. However it has no therapeutic potential and lesions identified will need treatment with the help of enteroscopy. When comparing more invasive forms of endoscopy (DBE) with capsule endoscopy, diagnostic rates are similar. Studies comparing DBE and capsule endoscopy have shown diagnostic yields of between 42.9–60% (for DBE) and 59.4–80% (for CE).Complete small bowel examination was achieved more frequently by capsule endoscopy. On the basis of the capsule findings, the clinician may proceed with push enteroscopy or double-balloon enteroscopy.
Push enteroscopy
The depth of insertion during push enteroscopy and the length of small bowel examined (30–160 cm) is variable The diagnostic yield of OGB with push enteroscopy is between 12 and 80%. with the highest yield in patients with overt bleeding. Push enteroscopy has proven value in the investigation of patients with suspected GI haemorrhage when initial conventional endoscopy is normal. However its use has declined with the advent of DBE.
Double Balloon Endoscopy (DBE)
The ability to confirm pathology and allow therapeutic application makes DBE complementary to CE. CE also helps in choosing the route of DBE. However DBE is labour intensive.
Intra Operative Endoscopy (IOE)
Historically, IOE has been considered the gold standard in patients with OGB and negative standard endoscopic evaluation. IOE should be reserved for patients with massive, continuous or recurrent gastrointestinal haemorrhage when other less invasive methods have failed to detect the source of bleeding. The reported techniques of IOE vary in several important aspects: approach to intra-abdominal access (laparotomy versus laparoscopy), enteroscope used and technique of insertion (per orally or via multiple enterotomies). The introductory route is chosen according to the location of the presumed pathology. The procedure is done jointly by the endoscopist and a surgeon.
Other investigations
The role of small bowel series, enteroclysis, cross-sectional imaging, and nuclear scans in the evaluation of obscure GI bleeding has declined substantially with the advent of capsule endoscopy because of its extremely low diagnostic yield.
Small-bowel follow-through and enteroclysis has been used to screen the small bowel for potential sources of bleeding, however the yield is very low.
CT enterography or MR enterography
These are newer imaging modalities that may be appropriately used in younger patients with suspected small bowel tumour.
Role of nuclear scans and angiogram
Neither tagged red blood cell scans nor angiography is useful in patients with obscure bleeding, because the blood loss often is too low to be detected.
Mesenteric angiography
Angiographic therapy is usually reserved for acutely bleeding lesions (equivalent to 3 units of blood loss per Day or > 0.5 ml/min) detected during diagnostic angiography. It has diagnostic yields of 40-44%, although yields as high as 74% have been reported. Angiography may be associated with significant morbidity, including renal failure, arterial dissection, ischemic colitis and death. Hence, given the high sensitivity and safety of other techniques (CE and DBE), angiography should be reserved for truly occult OGIB
Radioisotope bleeding scans
These are less invasive than angiography and may be helpful in cases of overt OGIB if the bleeding rate is in the range of 0.1 to 0.4 mL/min. These scans can aid in localization of the bleeding source, which can then be managed endoscopically, angiographically, or surgically.
Meckel’s scan
It is good for finding the diverticulum in young patients. However it is specific for Meckel’s only.
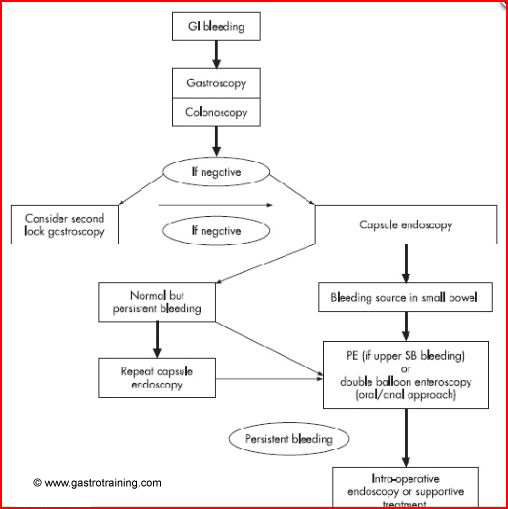
British Society of Gastroenterology algorithm for OGIB bleeds.
Ref