Nonalcoholic fatty liver disease (NAFLD) Nonalcoholic steatohepatitis (NASH)
What are NAFLD and NASH?
NAFLD is one of the common causes of elevated liver enzymes and chronic liver disease in the Western world. It is a clinico-histopathological entity with histological feature in keeping with alcohol related liver injury but with no/little history of excess alcohol consumption
It comprises of a spectrum ranging from simple steatosis to full blown steatohepatitis (NASH) that is characterized by steatosis, lobular inflammation, ballooning and fibrosis/cirrhosis.
Diagnosis of NAFLD requires:
- Liver biopsy showing steatosis, hepatocyte ballooning degeneration, mild diffuse lobular mixed acute and chronic inflammation, and perisinusoidal collagen deposition
- Alcohol consumption of less than 20g (equivalent units is 2.5units) of ethanol per week
- Absence of serologic evidence of hepatitis B or C or other pointers as to the aetiology e.g. autoimmune serology etc.
What is the burden of the problem?
- Data based on ultrasonographic studies and serum enzyme measurements indicate that the prevalence of NAFLD in the general U.S. population is approximately 30% and nearly 5 percent of children.
- There are no reliable data on the prevalence of NASH – the most severe form of NAFLD. However, a review of the literature suggests a prevalence of approximately 5 to 6%.
Discuss the natural history of the disease.
Steatosis alone is reported to have a more benign clinical course, with cirrhosis developing in only 1 to 3% of patients. However in patients with NASH, cirrhosis develops in 9 to 25%.
Discuss the clinical presentation of NAFLD/NASH?
Most patients are asymptomatic. Non specific symptoms like fatigue or vague RUQ abdominal discomfort frequently occur.
NAFLD is picked up on ultrasound examination requested for abdominal discomfort
NAFLD is also picked up by elevated ALT levels found incidentally.
GGT and alkaline phosphatase levels can be elevated too in NAFLD
Discuss evaluation of suspected NAFLD?
- The diagnosis of NAFLD requires that there is no history of previous or ongoing significant alcohol consumption (>21 U/week in males and >14 units/week in females). However lower amounts of alcohol may be toxic in individuals with metabolic risk factors such as obesity and diabetes.
- Low titres of ANA or SMA may be present in patients with NAFLD. However, liver biopsy should be considered to exclude autoimmune hepatitis if ANA is present in more than 1:160 titres and SMA at titres greater than 1:40.
- Raised serum ferritin is not uncommon. However, raised ferritin should prompt testing for HFE gene mutations.
- Chronic hepatitis B and hepatitis C should be excluded. Rare disorders like alpha-1 antitrypsin deficiency and Wilson’s disease should also be excluded in appropriate clinical setting.
- Medication history- medicines like tamoxifen, methotrexate, amiodarone etc can cause hepatic steatosis.
- NAFLD patients have significant co-morbidities like obesity, type2 diabetes and hyperlipidemia. These have prognostic significance.
How do you identify NASH in patients with NAFLD?
The NAFLD can be categorized into simple steatosis and steatohepatitis (NASH). Simple steatosis has a relatively benign course with minimal risk of progression to cirrhosis. However, NASH is histologically progressive and can lead to cirrhosis. It is thus important to distinguish NASH from simple fatty liver. Liver biopsy is the current gold standard to identify NASH.
Liver stiffness measured by transient elastography (FibroScan) may have some role in predicting the degree of fibrosis, but the data is limited in NAFLD. There has been significant research in developing biomarkers of liver histology in patients with NAFLD. Until more definite data with external validation become available, liver biopsy remain the gold standard.
What is the cause of insulin resistance associated with NAFLD?
- Increases in visceral adipose tissue and intrahepatic fat correlate with insulin resistance
- Insulin resistance may, at least in part, be related to substances secreted by adipocytes (“adipokines” including leptin, adiponectin, tumor necrosis factor alpha, and resistin)
- Some of these adipokines in particularly Leptin is produced by adipocytes and is secreted in proportion to adipocyte mass.
Discuss insulin resistance in the pathogenesis of fatty liver?
- Resistance to the action of insulin results in enhanced peripheral lipolysis and increased hepatic uptake of fatty acids leading to the accumulation of hepatocellular triglyceride.
- This in turn results in a preferential shift from carbohydrate to FFA beta-oxidation, an occurrence that has been demonstrated in patients with insulin resistance.
- FFAs are inducers of several cytochrome p-450 microsomal lipoxygenases, capable of producing hepatotoxic free oxygen radical species.
- Furthermore, the shift to FFA beta-oxidation may also result in increased free radical formation, hepatocellular injury, and fibrosis.
Discuss insulin resistance and atherosclerotic cardiovascular disease?
Insulin resistance, the associated hyperinsulinemia and hyperglycemia, and adipocyte cytokines (adipokines) may also lead to
a. vascular endothelial dysfunction,
b. an abnormal lipid profile,
c. hypertension, and
d. vascular inflammation,
All of which promote the development of atherosclerotic cardiovascular disease (CVD)
This is important because patients with NAFLD have a high incidence of cardiovascular morbidity and mortality. Several longitudinal studies have shown that cardiovascular disease is much more common than liver disease as a cause of death in patients with NAFLD.
What is metabolic syndrome or syndrome X?
Any patients meeting three of the five criteria
- Glucose >= 5.6mmol/L or drug treatment for elevated blood glucose
- HDL cholesterol <1.0mmol/L in men and <1.3mmol/L in women or drug treatment for low HDL-C
- Triglyceride >= 1.7 mmol/L or drug treatment for elevated triglycerides
- Obesity Waist 102 cm (men) or 88 cm (women)
- Hypertension 130/85 mmHg or drug treatment for hypertension
How fat causes liver disease?
- FFAs are inducers of several cytochrome p-450 microsomal lipoxygenases, capable of producing hepatotoxic free oxygen radical species.
- Furthermore, the shift to FFA beta-oxidation may also result in increased free radical formation, hepatocellular injury, and fibrosis.
- Perisinusoidal (zone 3) fibrosis in patients with NASH is a consequence of the activation of lobular stellate cells.
- Portal fibrosis is commonly a feature of progressive disease. It stems from the activation of a secondary replicative pathway involving hepatic progenitor cells (HPCs)
What is the two-hit theory in NAFLD?
- FIRST HIT is the insulin resistance, which leads to hepatic steatosis.
- It is not clear why some patients with hepatic steatosis progress to nonalcoholic steatohepatitis and most do not. It is proposed that a SECOND HIT, in the form of oxidative stress leads to chronic necroinflammation in the liver.
- Free radical formation, Hepatic iron overload, cytokine release, leptin, antioxidant deficiency and impaired mitochondrial energy production -all have been suggested as potential oxidative stressors.
Can NON obese patients get fatty liver?
Yes.
- Even a minor accumulation of adipose tissue in the abdominal region in non-obese men could be associated with a considerably adverse metabolic risk profile
Richelsen B et al :Int J Obes Relat Metab Disord 1995 Mar;19(3):169-74.
- Available evidence also suggests that MONW (The metabolically obese, normal-weight) individuals could account for the higher prevalence of type 2 diabetes, cardiovascular disease, and other disorders in people with a BMI in the 20-27 kg/m2 range who have gained modest amounts of weight (2-10 kg of adipose mass) in adult life.
Ruderman N et al, Diabetes 1998 May;47(5):699-713.
NAFLD may be associated with a variety of clinical conditions. Discuss
- Obesity- 69 to 100 percent of cases of NASH
- Type 2 DM- 34 to 75 percent of patients of NASH
- Hyperlipidaemia- 20 to 80 percent of patients of NASH
- TPN
- Rapid weight loss
- Acute starvation
- Abdominal surgery like jejunal bypass, bariatric operation
- Drugs e.g. steroid, amiodarone, tamoxifen, HAART
- Misc e.g. abetalipoproteinaemia, Wilson’s disease, jejunal diverticulosis with bacterial overgrowth
Who needs liver biopsy?
Liver biopsy remains the gold standard to establish the diagnosis of NAFLD. It is also the only accurate method to stage fibrosis in the liver. However, in the absence of effective therapy and the significant prevalence of NAFLD, the decision to perform liver biopsy for diagnosis and staging of fibrosis remains controversial.
However, consider liver biopsy strongly if
- Clinical evidence of chronic liver disease or portal hypertension (splenomegaly, cytopenias)
- Abnormal iron studies
- ANA or SMA in significant titres
- Diabetes and/or significant obesity in an individual over the age of 45 (these factors are associated with an increased risk of significant fibrosis)
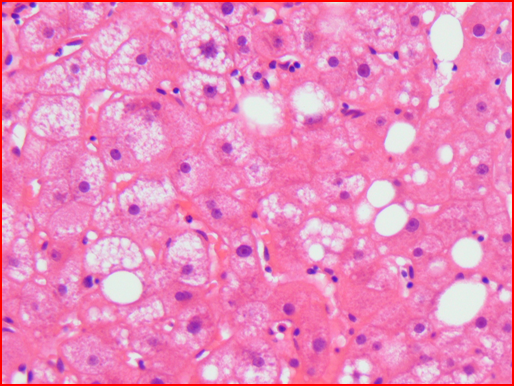
Discuss the histological findings in NAFLD?
- Microvesicular steatosis
- Macrovesicular steatosis
- Mallory bodies- eosinophilic accumulations of intracellular material
- Ballooning degeneration
- Perisinusoidal zone 3 fibrosis
- Scattered, predominantly lobular, neutrophilic or mixed inflammation
Histology of NASH: Showing micro and macrovesicular steatosis
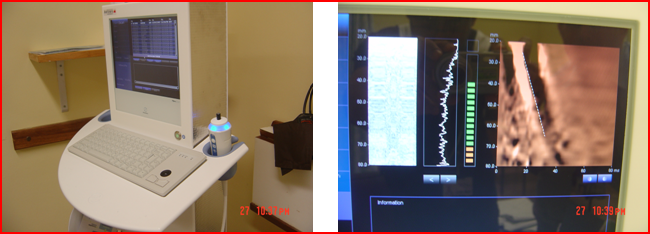
What is FibroScan?
- FibroScan use an ultrasonic transducer to send a vibration of low frequency (50 MHz) and amplitude into the liver.
- The vibration wave induces an elastic shear wave that propagates through the organ.
- The velocity of this wave correlates directly with tissue stiffness- the stiffer the tissue the faster the wave
- Results are expressed in kilopascals (kPa). Normal value is less than 7
FibroScan unit and the standard picture
Discuss the management of NAFLD?
- It is generally believed that weight loss is beneficial for patients with NAFLD, but data is limited in terms of specifics such as how, how much and how rapidly to lose weight.
- Role of bariatric surgery: liver histology improves significantly following bariatric surgery. Bariatric surgery may be used as a therapeutic possibility for the severely obese NAFLD patients with advanced fibrosis who fails to lose weight by conventional means.
- Role of insulin sensitizers- insulin resistance is nearly universal in patients with NASH.
- A recent meta-analysis showed that metformin leads to normalization of serum aminotransferases in a significantly greater proportion of patients compared to dietary modification and improved steatosis by imaging. The role of Metformin in diabetic patients with NASH is unknown
- Thiazolidinediones (TZD) – rosiglitazone and pioglitazone. TZDs have a favourable effect on liver biochemistries and histology. However, long term treatment is needed to maintain their therapeutic benefits. This is potentially a significant issue as recent studies questioned the long term safety of TZDs.
- Some hepatologists are already using insulin sensitizing drugs ( metformin 850 mg twice daily or pioglitazone 45 mg daily) based upon the preliminary data
- Patients with NAFLD have a high incidence of cardiovascular morbidity and mortality. Several longitudinal studies have shown that cardiovascular disease is much more common than liver disease as a cause of death in patients with NAFLD. Thus it is important to emphasize the significance of cardiovascular disease to patients with NAFLD and their primary care providers. Statins remain a cornerstone for managing dyslipidemia and coronary artery disease.
Given the slow rate of progression in most patients with NASH, currently control of risk factors rather than medical therapy is recommended in most patients.
In summary:
- There is currently no medical treatment that reverses fatty liver disease and causes fat within the liver to resolve.
- A few studies have suggested that weight loss may be associated with regression of fat within the liver-
- Treatment of NAFLD- control of metabolic risk factors rather than medical treatment is recommended.
Ref