Chronic Pancreatitis (CP)
Discuss chronic pancreatitis?
Chronic pancreatitis is the progressive and permanent destruction of the pancreas resulting in exocrine and endocrine insufficiency and, often, chronic disabling pain.
Discuss the aetiology of CP?
The aetiology is multi factorial. Chronic alcohol use accounts for 70 percent of the cases
of chronic pancreatitis in adults. Idiopathic chronic pancreatitis accounts for 20%. The rest 10% is accounted by
- Genetic causes (mutations in the cystic fibrosis gene, hereditary pancreatitis)
- Ductal obstruction (e.g., post traumatic pancreatic duct fibrosis, pseudocysts, stones, tumours, possibly pancreas divisum)
- Tropical pancreatitis
- Systemic disease such as SLE, hypertriglyceridemia, possibly hyperparathyroidism
- Autoimmune pancreatitis
Discuss the clinical features of CP?
Patients may have recurrent episodes of acute pancreatitis, which can progress to chronic abdominal pain. The ‘‘classic’’ pain is located in the epigastrium, radiates to the back, is associated with oral intake, nausea, vomiting, and is relieved by sitting forward. In some patients there is a spontaneous remission of pain by organ failure (pancreatic burnout theory).
About 10- 20% of patients with chronic pancreatitis present with endocrine or exocrine dysfunction in the absence of abdominal pain. Exocrine dysfunction leads to maldigestion causing patients to present with diarrhoea, steatorrhoea, and weight loss. Steatorrhoea typically occurs before protein deficiencies. Malabsorption of fat soluble vitamins and cobalamin (vitamin B12) may occur, although clinically significant vitamin deficiency is rare.
Discuss the investigations for CP?
Large duct disease, most commonly associated with alcohol misuse, is well recognised by most physicians and diagnosed comparatively easily as virtually any diagnostic test will show large duct chronic pancreatitis. The typical tests used to diagnose large duct disease are often too insensitive to diagnose small duct disease.
- Pancreatic enzymes may be elevated during episodes of acute pancreatitis; however, in most cases, serum amylase and lipase levels may be normal or only mildly elevated.
- USS- rarely diagnostic
- Contrast enhanced CT scan is the Initial radiologic test of choice for evaluation of suspected chronic pancreatitis; Pathognomonic findings on plain radiography and CT reveal calcifications within the pancreatic ducts
- EUS- It should be considered in patients with normal imaging tests but high degree of suspicion for chronic pancreatitis. EUS alone however may overestimate disease because many of the early endoscopic changes with chronic pancreatitis can be identified in normal aging. Thus EUS diagnosis of early pancreatitis is not secure unless it is complemented by a positive secretin test.
- ERCP- it is the reference standard in many studies. It is mainly used in diagnosis of early chronic pancreatitis with normal computed tomography and pancreatic function test.
- MRI or MRCP- less sensitive than ERCP for evaluation of side branches; can be combined with secretin test.
- Pancreatic function tests- The secretin stimulation test is the most sensitive and specific testing available for the diagnosis of chronic pancreatitis. However it is not available widely. (A collection tube is placed in the 3rd part of duodenum under fluoroscopic guidance. After a test dose (0.2 mcg) of synthetic secretin, a full dose (0.2 mcg/kg) is administered as an intravenous bolus at time 0. Duodenal fluid is continuously collected in 15 minute aliquots for one hour. A bicarbonate concentration less than 80 mEq/L in all of the four aliquots represents exocrine insufficiency).
- Faecal elastase- is the test of choice in patients with symptoms of malabsorption.
Discuss the treatment of CP?
Pain control
The pathogenesis of the pain remains poorly understood, but has been thought to be associated with perineural inflammation, increased pressure in both large and small ducts, and in the pancreatic parenchyma, an abnormal feedback mechanism, or pancreatic carcinoma with duct obstruction. Management of pain:
- Cessation of alcohol use.
- Low fat small meals
- Pancreatic enzyme supplements relieve pain in some patients. Mechanism- In a subset of patients it seems that the pancreas is under constant stimulation by CCK.A CCK releasing peptide has been identified that resides in the proximal small intestine and is degraded by the serine proteases. As patients with chronic pancreatitis have decreased protease activity they may be unable to inactivate this releasing enzyme leading to perpetual pancreatic stimulation. These patho-physiological mechanisms illustrate the importance of exogenous protease to allow the pancreas to rest and afford pain relief. To achieve feedback inhibition and thus have an impact on pain it is necessary to deliver exogenous protease to the proximal small intestine (i.e. use non enteric coated enzyme supplements plus PPI) as the serine proteases and CCK peptide are found there. A regimen of non-enteric coated enzymes taken orally with meals and at bedtime provides good clinical response in most patients. Certainly the greatest success is seen in patients with small duct disease.
- Analgesics — Analgesia can be considered if pancreatic enzyme therapy fails to control pain. Use paracetamol and NSAIDS first. If not effective try tramadol or codeine. Chronic opiods analgesia may be required in patients with persistent significant pain. Long-acting agents such as morphine sulphate continuous release or fentanyl patches are generally more effective than short acting medications, which last only three or four hours.
- Octreotide- inhibits pancreatic secretion and considerably lowers CCK levels. A multicentre pilot study was performed in 1993 to examine various dosing regimens and showed that 200 mg of octreotide taken subcutaneously three times daily was superior to placebo. Octreotide significantly relieves pain in many patients with severe chronic pancreatitis that is refractory to other forms of therapy. Predictors of response remain unclear at this time, but it probably acts through reduction in CCK levels.
- EUS guided coeliac axis block (with bupivacaine) represents a comparatively safe and well tolerated option in the treatment of chronic pancreatitis pain. However it is invasive with only short term benefits and thus has a limited application.
Steatorrhoea and malabsorption
Patients do not develop steatorrhoea until their lipase level decreases to less than 10% of normal. This is treated with pancreatic enzyme supplements.
Role of ERCP
Endoscopic pancreatic duct decompression via ERCP has been found to give pain relief in some patients. The principle behind this approach is that by decreasing ductal pressure as seen in pancreatic duct strictures, pain relief can be attained. Obstruction of the pancreatic duct can be secondary to stricture, stones or both. Endoscopic intervention consists of pancreatic duct stricture dilatation, stent placement, stone extraction, or pancreatic duct sphincterotomy.
Surgery
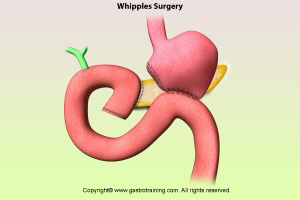
Surgical decompression is typically considered in refractory pain in the presence of pancreatic ductal dilatation > 6 mm secondary to technical issues. Decompression procedures are used in patients with large duct disease. Lateral pancreaticojejunostomy is commonly performed and yields pain relief in 60 to 91 percent of patients; recent studies have found it to be more effective than endoscopic drainage for long-term pain relief.
Resective procedures are considered in patients with pancreatic mass or small duct disease. Resective procedures include pancreatoduodenectomy (Whipple procedure, pylorus-preserving, and duodenum-preserving) and distal or total pancreatectomy. The Whipple procedure has been the most widely performed surgery in patients with chronic pancreatitis. It provides pain relief in 85 percent of patients, with mortality rates of less than 3 percent. Distal pancreatectomy is associated with an increased risk of early-onset diabetes and is only indicated if the disease is confined to the tail of the pancreas. Total pancreatectomy is a last-resort procedure associated with a high rate of brittle diabetes and inadequate pain relief and, therefore, should be accompanied by autologous islet cell transplantation. Patients should be counselled about inadequate pain relief, complications, and increased rate of exocrine and endocrine insufficiency before proceeding with surgery.
Discuss the complications of CP?
- Diabetes
- Pseudocysts- Most pseudocysts are asymptomatic, but they can cause complications in 25 to 30 percent of patients and can result in rupture, infection, intracystic bleeding, and obstruction of the surrounding structures.
- Portal hypertension and gastric varices result from thrombosis of the splenic vein; this can cause pseudoaneurysms to form, especially in the splenic artery.
- Episodes of acute pancreatitis can cause pancreatic abscesses, necrosis, sepsis, and multiorgan failure.
- There is a 15-fold risk of pancreatic cancer for patients with chronic pancreatitis who are alcoholics and a 40 percent lifetime risk for those with hereditary disease.
- Bile duct, duodenal or gastric obstruction
- Pancreatic ascites or pleural effusion
Ref