Cancer Surveillance in IBD
Discuss cancer surveillance in IBD?
- Patients with IBD are at an increased risk of colorectal cancer (CRC).
- The risk is related to the anatomic extent and duration of disease.
- Patients with proctitis and proctosigmoiditis are probably not at an increased risk of CRC.
- An increased risk of CRC has been observed in patients with UC complicated by PSC. Cancer always occurs in chronically inflamed areas.
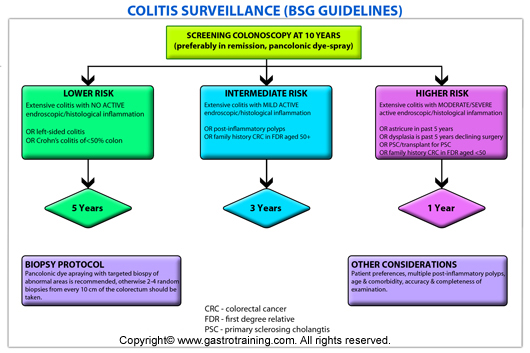
- The American Gastroenterological Association (AGA) concluded that the risk of colorectal cancer associated with ulcerative colitis and Crohn’s colitis is similar for comparable extent and duration of disease. As a result, the surveillance strategy for UC also applies for Crohn’s colitis. The British Society of Gastroenterology (BSG) recommends the same.
Left sided colitis: Involvement limited to a proportion of the colorectum distal to the splenic flexure
Extensive colitis: UC extending proximal to the splenic flexure or Crohn’s colitis affecting at least 50% of the surface area of the colon.
Discuss the AGA recommendations for cancer surveillance in IBD?
Colonoscopic surveillance should begin after eight years in patients with pancolitis, and 15 years in patients with colitis involving the left colon. Colonoscopy should be repeated every one to two years.
Does colonoscopic surveillance reduce mortality?
No large controlled trials have proven that surveillance reduces mortality.
Discuss the biopsy protocol?
The optimal number and location of biopsies that should be obtained is uncertain. In one study, Rubin et al (Gastroenterology 1992) reported that 33 biopsy specimens would be required to detect dysplasia with 90 percent confidence. The BSG recommends two to four random biopsy specimens every 10 cm from the entire colon, with additional samples of suspicious areas. American Society for Gastrointestinal Endoscopy (ASGE) recommends four biopsies should be obtained every 10 cm from the caecum to the rectum. In addition, any suspicious lesions or masses should be biopsied.
Chromoendoscopy (pan colonic dye spraying) has been recommended as the technique of choice for cancer surveillance in colitis. Narrow band imaging has been shown to be no better than white light colonoscopy in a study.
Discuss dysplasia and IBD surveillance?
It is generally believed that CRC in IBD is preceded by dysplasia. Histologically, dysplasia is classified as negative, indefinite and positive (low and high grade). Dysplastic areas are difficult to recognize on endoscopy. They may appear as flat or only slightly elevated above the level of the mucosa.
What is the predictive value and treatment of dysplasia?
Berstein (Lancet 1994) did a very nice study- collating a total of ten prospective colonoscopic surveillance studies that had 1225 patients. Those individuals that had
No dysplasia 2% would go on to develop HGD/ DALM /carcinoma
indefinite 18% HGD/ DALM /carcinoma.
LGD 29% HGD/ DALM /carcinoma
HGD 33% develop carcinoma
There is general consensus that high-grade dysplasia warrants colectomy because of the high rate of synchronous CRC.
The management of low grade dysplasia is more controversial, but a colectomy is generally recommended. If the patient with LGD is unwilling to undergo colectomy, BSG recommends yearly surveillance. If there is any uncertainty about the diagnosis of LGD, a repeat colonoscopy within 3 months using chromoendoscopy should be done.
It is important to remember that although dysplasia is a marker for future or concurrent malignancy, it can also regress or remain stable for long periods.
What is a DALM and what is its significance?
Dysplastic polyps arising within an area of inflammation have been term dysplasia-associated lesions/masses (DALMs).
It is essential to biopsy the flat mucosa surrounding any dysplastic polyp to assess the extent of disease (as it may not be apparent macroscopically) and also to assess whether there is any dysplasia in the surrounding ?at mucosa.
Possibilities:
If a dysplastic polyp occurs in an area proximal to the microscopic level of in?ammation, with no dysplasia in ?at mucosa, it can be regarded as a sporadic adenoma and treated accordingly.
If a dysplastic polyp is arising within a ?eld change of dysplastic tissue in the surrounding ?at mucosa, colectomy should be recommended as full excision of the lesion will not be possible endoscopically.
If a dysplastic polyp is detected within an area of in?ammation but can be removed in its entirety, it is usually not necessary to recommend colectomy. However, if the dysplastic polyp cannot be completely excised, either urgent re-assessment of resectability by an experienced colonoscopist or urgent surgery is required irrespective of the grade of dysplasia.
Discuss chemoprevention?
Current evidence suggest that aminosalicylates reduces the risk CRC in IBD patients. BSG recommends that patients are kept on aminosalicylates at a dose of at least 1.2 g/day for chemoprevention.
Ref






