Surgery in Ulcerative Colitis
Discuss the indications for surgery in UC?
- Persistent symptoms despite medical therapy
- Steroid dependent disease
- Dysplasia/malignancy
Discuss the types of surgery in UC?
Since UC only affects large bowel, a proctocolectomy is curative. Further ileal pouch surgery allows patients to live without ileostomy. Surgical options are:
- Proctocolectomy with ileostomy
- Total colectomy with ileorectal anastomosis
- Colectomy, mucosal proctectomy, and ileal pouch-anal canal anastomosis (IPAA)
- Colectomy and stapled ileal pouch distal rectal anastomosis (IPDRA)
Total colectomy with ileostomy is the procedure of choice in emergency situations. Subsequent proctectomy with ileal pouch-anal anastomosis can be done electively. IPAA has high complication rates when performed on patients with acute/toxic colitis.
Further, ileostomy may also be needed if IPAA is not technically possible or has failed. Most patients’ small bowel will extend the necessary length, and a variety of techniques are employed to make the ileum reach the anal canal. In the unusual event that the small bowel does not reach, a permanent ileostomy may be needed.
Ileorectal/IPDRA anastomosis is technically easier surgery than IPAA. Further it leaves the rectal mucosa behind. This may cause persistence of symptoms and future risk of malignancy. The ileorectal anastomosis has the advantage of better continence, especially at night. This operation may be considered in:
- Pts with minimal rectal involvement and not suitable for IPAA but refuse ileostomy or where stoma is relatively contraindicated (e.g. ascites)
- Some advocate the operation in women of child bearing age because of the risk of infertility with IPAA
- It may also be a good choice for patients in whom Crohn’s disease cannot be excluded. IPAA is usually avoided in patients with Crohn’s disease because of poorer functional outcomes and a higher failure rate.
Discuss the complications of pouch surgery?
- Early complications- The most common complications include small bowel obstruction (17–20%), wound infections (5.8%), and bleeding (3.8%). Other complications- anastomotic leak, portal vein thrombosis
- Late complications
- Anastomotic stricture.
- Fistula and abscess
- Pouchitis- chronic pouchitis occurs in 10%.
- Irritable pouch syndrome
- Reduced fertility
- Anorectal dysfunction (anismus).
- Pouch failure- (defined as removal of the pouch or the need for an ileostomy) 7-13% at 10 years. Commonest cause is fistula
- Post pouch- Mean no of stools at 5 years-Day-(6 + 2), night (2+1). Major nocturnal incontinence is 22% over 10 years
Discuss pouch surgery and pregnancy?
Pregnancy and delivery are safe in patients with IPAA. Whether vaginal or Caesarean delivery is better remains controversial. The type of delivery should be influenced by obstetric consideration but also the potential risk of sphincter injury. Some have favoured Caesarean sections
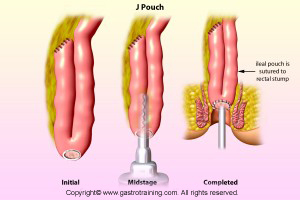
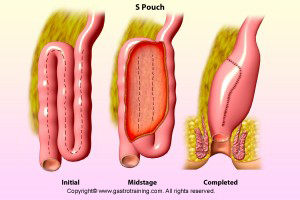
Discuss the types of pouch?
The J, S and W reservoirs are the most common types of pouches used. Selection of pouch design depends on a variety of factors, including age, patient size and individual anatomy.