Constipation
Discuss the diagnostic criteria for constipation?
At least 12 weeks (need not be consecutive) in the preceding 12 months of 2 or more of-
- Straining in >¼ defecations
- Lumpy or hard stools in >¼ defecations
- Sensation of incomplete evacuation in >¼ defecations
- Sensation of anorectal obstruction/blockade in >¼ defecations
- Manual maneuvers to facilitate >¼ defecations (e.g., digital evacuation, support of the pelvic floor) and/or <3 defecations/week
- Loose stools are not present, and there are insufficient criteria for IBS
Constipation is clearly very common. The role of the gastroenterologist is to assist in identifying selected patients with constipation who might benefit from additional testing or more specific treatments.
Discuss the disorders of colonic motility and constipation?
Constipation is the major feature of 2 disorders of colorectal motility.
- Slow Transit Constipation (STC) – is thought to have as a primary defect slower than normal movement of contents from the proximal to the distal colon and rectum.
- Pelvic floor dysfunction (outlet obstruction) - normal or slightly slowed colonic transit overall but a preferential storage of residue for prolonged periods in the rectum. In this instance, the primary failure is one of an inability to evacuate adequately contents from the rectum. The simplest possible classification would subdivide evacuatory failure into the following: (a) examples of muscular hypertonicity (failure to relax); incomplete relaxation or paradoxical contraction of the pelvic floor and external anal sphincters during attempted defecation and (b) muscular hypotonicity, sometimes with megarectum and excessive pelvic floor descent. These syndromes are multifactorial, and some are not yet well understood.
- Combination of the two- separation of STC from disorders of evacuation as the major cause of constipation is extremely important because the primary therapeutic approaches differ significantly.
Discuss the clinical evaluation of constipation?
- IBS- strong emphasis on symptoms that occur between infrequent bowel movements (bloating, pain, malaise) suggests an underlying IBS.
- Patients with significant pain are more likely to have normal gastrointestinal transit than those with painless constipation
- Prolonged and excessive straining before elimination is suggestive of pelvic floor dysfunction. The need for perineal or vaginal pressure to allow stools to be passed or direct digital evacuation of stools is even stronger clues.
What are the common medical conditions associated with constipation?
- Drugs esp. opiods
- Mechanical obstruction- cancer, stricture (diverticular/ischaemic), rectocele, anal fissure, megacolon
- Metabolic- hypothyroid, diabetes, hypercalcemia, hypokalemia, hypomagnesemia, uremia, heavy metal poisoning
- Myopathies- scleroderma, amyloidosis
- Neuropathies- CVA, MS, spinal cord lesions, Parkinsons disease
- Others- depression, immobility, autonomic neuropathy, cardiac disease
Discuss the investigations to evaluate constipation?
Patients who fail to respond to simple medical treatment after excluding contributing causes are appropriate candidates for more specialized testing. A simple, inexpensive radiopaque marker study will identify STC. Pelvic floor dysfunction needs to be excluded by performing anorectal manometry; if confirmed, defecography will solidify the diagnosis and evaluate anatomic defects.
- Most patients (particularly pts aged >50) will require structural studies (barium enema or colonoscopy) and blood chemistries to exclude metabolic disorders.
- Colonic transit- The method most commonly used to measure transit is that of radiopaque markers (SHAPE study). Severely constipated patients should have laxatives/enemas to empty the colon before a study of transit as rectal distension by retained stool can slow colonic transit. Adults ingest a capsule (containing 20 markers or shapes) and an AXR is taken on day 5. If more than 20% of the rings are counted on the x-ray, delayed colonic transit is present.
- In pelvic dyssnergia- the markers may concentrate on the left colon or rectosigmoid junction. However 2/3 of pts with pelvic dyssnergia will have markers retained throughout the colon. Also 1/3rd of pts with pelvic dyssergia may have normal SHAPE study. Thus SHAPE study is useful for diagnosing STC only. If pelvic dyssnergia is suspected, manometry should be requested.
- Defecography- Barium defecography can be performed in conjunction with a standard barium enema (for structural evaluation of the whole colon), and thus an anatomic/functional evaluation of defecation can be performed at the same time. The most relevant observations are (a) the failure of the anorectal angle to open (i.e., become more obtuse) during defecation and (b) the degree of pelvic floor descent during defecation. Decreased descent is a component of impaired pelvic floor relaxation (“anismus”), and, conversely, excessive descent (“descending perineum syndrome”) can also be a pathophysiologic mechanism of constipation.
- Anorectal manometry- The procedure has greatest value in (1) excluding Hirschsprung’s disease by the presence of a normal rectoanal inhibitory reflex and (2) providing supportive data for clinical or physiologic suggestions of pelvic floor dysfunction. For example, high basal sphincter pressures with relatively little voluntary augmentation, suggest spastic pelvic floor/sphincter dysfunction
Discuss the management of STC?
Normal transit constipation- can be treated with fiber and/or laxatives.
Slow transit constipation-
- Step 1- use laxatives as above.
- Step 2- If the response is poor the colonic transit study could be repeated on laxative medications. If the transit study is normal- the medications could be adjusted.
- Step 3- However if the transit study is still abnormal, repeat tests for pelvic dysfunction should be done. If there is no evidence of dyssynergia, surgery could be considered.
Surgical treatment of STC- Total colectomy with ileorectal anastomosis can be considered when medical treatment has failed. Patients need to be told that the procedure is designed to treat the symptom of constipation (difficult and infrequent evacuation) and that other symptoms (e.g., abdominal pain and bloating) that the patient associates with constipation may not necessarily be relieved by achieving regular defecation.
Before surgery it is vital to exclude dyssynergia and if present should be treated before surgery or else ileostomy considered. The contraindication to surgery is presence of upper GI or diffuse motility disorder. Patients who continue to be constipated after ileorectostomy are likely to have abnormal pelvic floor function.
Discuss the management of constipation due to pelvic floor dysfunction?
- Step 1- laxatives (response may be poor)
- Step 2- biofeedback- if no improvement-
- Step 3- repeat tests for pelvic floor dysfunction- if normal begin normal transit constipation algorhithm but if abnormal
- Step 4- define anatomic rectal defect- if clinically significant- surgery. If defect not significant- reassess biofeedback and laxatives- if still not effective- consider surgery to repair the defect.
Pelvic floor retraining- Biofeedback and relaxation training have been quite successful and, importantly, free of morbidity. Biofeedback can be used to train patients to relax their pelvic floor muscles during straining and to correlate relaxation and pushing to achieve defecation. By the relearning process, the nonrelaxing pelvic floor is gradually suppressed and normal coordination restored. Intensive programs in adults can have a 75% success rate or better.
Discuss the laxatives used for constipation?
- Stimulant laxatives- bisacodyl (dulcolax) 5mg tab 1-2 nocte, Co-danthramer, sodium decussate, senna, sodium picosulphate (Dulcolax perles capsules) 5mg caps- 2-4 at night.
- Osmotic laxatives- lactulose, magnesium salts- milk of magnesia- 25-50 mls prn, Milpar- 5-20mls prn, Andrews liver salts (MgSO4), macrogols or PEG- movicol. These laxatives all have the same mechanism of action i.e. osmotic retention of fluid in the gut lumen.
Discuss Prucalopride in the treatment of constipation in women?
Prucalopride (Resolor, Movetis) is a selective serotonin (5-HT4) receptor agonist that predominantly stimulates colonic motility. Prucalopride is administered orally.
Dose: recommended dose of prucalopride is 2 mg once daily for adult women (up to 65 years old) and 1 mg once daily for older women (over 65 years). The dose for older women can be increased to 2 mg once daily if needed. If once-daily prucalopride is not effective after 4 weeks, the patient should be re-examined and the benefit of continuing treatment reconsidered.
Side effects: most common adverse effects include headache and gastrointestinal symptoms (abdominal pain, nausea or diarrhoea). Most adverse effects occur at the start of treatment and usually subside within a few days of continued treatment.
NICE 2010 recommends prucalopride as an option for the treatment of chronic constipation only in women for whom treatment with at least two laxatives from different classes, at the highest tolerated recommended doses for at least 6 months, has failed to provide adequate relief and invasive treatment for constipation is being considered. NICE further recommends that if treatment with prucalopride is not effective after 4 weeks, the woman should be re-examined and the benefit of continuing treatment reconsidered.
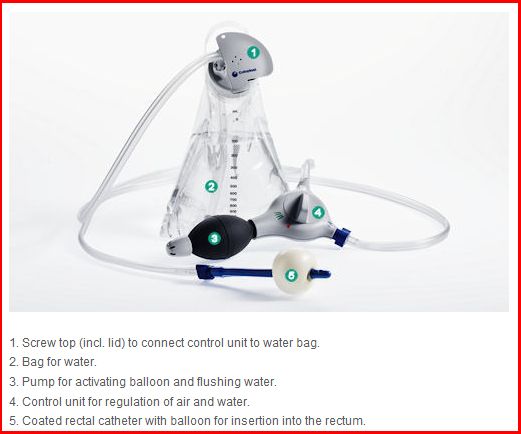
Anal irrigation
Anal / rectal irrigation may be an appropriate form of management for people suffering from chronic constipation. An anal irrigation system will contain everything you need to irrigate your bowels. An anal irrigation system will usually consist of a control unit with a pump, a water bag and a rectal catheter.
For further information about the Peristeen anal irrigation system, please visit www.coloplast.co.uk
Peristeen Anal Irrigation works by introducing luke warm tap water into the bowels using a rectal catheter.
Principle:
The principle behind the system is very simple. Peristeen Anal irrigation is performed by introducing lukewarm tap water into the rectum using a rectal catheter, whilst sitting on the toilet. The water fills up in the large intestine and causes the faeces to move onwards in the bowel. After introducing the appropriate amount of water (usually 500-1000ml) into the bowels, water and stools are emptied into the toilet.
Anal irrigation is an alternative to other methods such as laxatives, suppositories and mini enemas.
Peristeen anal irrigation system
Please see the User guide video here
Risks:
Bowel perforation is an extremely rare (less than one in 100,000 uses) complication to anal irrigation (see recent MHRA alert)
MHRA recommendation:
Ensure that patients (and where appropriate carers):
- have received comprehensive training and are competent in the use of the system before using it unsupervised
- are aware of the risk of bowel perforation, how to recognise the symptoms and actions to be taken ( contact your doctor, if you have Severe and sustained abdominal pain or back pain, especially if combined with fever or have Sustained anal bleeding)
Before starting Peristeen Anal Irrigation, Coloplast instruct that patients should undergo a medical evaluation by a doctor with appropriate expertise to ensure that they have no conditions that preclude its use or require further investigation.
Contraindications:
Peristeen Anal Irrigation must not be used in the following situations:
- Known obstruction of the large bowel due to strictures or tumours.
- Acute inflammatory bowel disease.
- Diverticulitis.
- Complex diverticular disease
- Recent abdominal or anal surgery
Peristeen Anal Irrigation is not recommended for:
- Children under 3 years of age ((as it contains phthalate: dibutyl phthalate)
- Pregnant or nursing women (as it contains phthalate: dibutyl phthalate)
Special caution must be shown if you have or have had any of the following:
- Any anorectal condition, which may cause pain or bleeding e.g. anal fissure, severe haemorrhoids (third or fourth degree haemorrhoids).
- Irradiation therapy in the abdominal or pelvic region.
- Recent colonic biopsy.
- Spinal cord shock phase.
- Autonomic dysreflexia.
- Cancer in the abdominal or pelvic region.
- Long term steroid therapy.
- Anticoagulant therapy.
- Changed stool pattern like sudden diarrhea of unknown origin. The cause for diarrhea must be identified.
- Rectal medication for other diseases. The effect of such medication may be diluted by the anal irrigation.
- Risk factors for ischaemic colitis (atrial fibrillation, coronary artery disease, hypercholesterolaemia).
- Onset of any the above mentioned conditions.
- Blood in faeces, weight loss, abdominal pain.
- Changes in the frequency, colour and consistency of the stools.
Ref