LARGE BOWEL
Discuss the various parts of large bowel?
Colon is about 1.5 m long. The large bowel is distinguished from small intestine by its three thickened band of longitudinal muscles (taenia coli) and the sacculations on its wall, between the taenia, called haustra. Haustra are formed because taenia is shorter than the large bowel
The parts of the large bowel are:
| Anatomy | Arterial supply | Lymphatic drainage | |
| Caecum | 5-7 cms long. Ileum and appendix open in it, Entirely covered by peritoneum |
Ileocolic branch of superior mesenteric artery | Ileocolic nodes and then to superior mesenteric nodes |
| Ascending colon | 12-20cms, retroperitoneal | Ileocolic and right colic branches of superior mesenteric artery | Paracolic and epicolic nodes and then to superior mesenteric nodes |
| Transverse colon | 45 cms, largest and most mobile part. It has a mesentery called transverse mesocolon | Middle colic artery branch of superior mesenteric artery. Also supplied by right and left colic artery | Nodes along middle colic artery and then to superior mesenteric nodes |
| Descending colon | 22-30cms, retroperitoneal | Left colic and superior sigmoid branches of inferior mesenteric artery | Intermediate colic nodes along left colic artery and then to inferior mesenteric nodes. Splenic flexure also drains to superior mesenteric nodes |
| Sigmoid colon | 40 cms, extends from pelvic brim to S3, has a long mesentery- sigmoid mesocolon | Sigmoid artery branches of inferior mesenteric artery | Intermediate colic lymph nodes along the left colic artery and then to inferior mesenteric nodes |
| Rectum | 12-15 cms, peritoneum covers the superior 2/3 rd of the rectum. The inferior 1/3 rd has no peritoneal covering. Terminal part of rectum has an anterior dilatation called ampulla. | Superior part of rectum- Superior rectal artery (continuation of inferior mesenteric artery) Middle and inferior parts- supplied by two middle rectal arteries, branches of internal iliac artery Inferior part of rectum- two inferior rectal arteries, branches of internal pudendal artery |
Superior half of rectum- pararectal nodes and then to inferior mesenteric nodes and aortic nodes
Inferior half of rectum- internal iliac nodes |
| Anal canal | 4 cms long, Pectinate line (dentate line, mucocutaneous line) is the junction of columnar epithelium of the superior part of anal canal and the stratified squamous epithelium of the inferior part. In surgical usage, however, the anal canal is frequently limited to that part of the intestine below the dentate line. |
Superior rectal artery supplies the anal canal above the dentate line Two inferior rectal arteries supply the anal canal below the dentate line. The unions of the superior with the middle and inferior rectal veins are important portal-systemic anastomoses. |
Internal iliac nodes from superior to the dentate line Superficial inguinal nodes- inferior to the dentate line |
Discuss the relations of rectum?
Anteriorly- the rectovesical pouch and bladder in males. Uterus, cervix and vagina in females
Laterally- ischial tuberosity and spine
Posteriorly- sacrum and coccyx
Discuss haemorrhoids and anal sphincters?
Internal haemorrhoids are varicosities of the branches of superior rectal veins and covered by mucous membrane and external haemorrhoids are varicosities of the branches of inferior rectal veins and are covered by skin
Anal sphincters- Anal canal has an external and internal sphincters- both must relax before defecation can occur. The external sphincter is voluntary and surrounds the inferior 2/3rd of the anal canal. The internal sphincter is involuntary and surrounds the superior 2/3 rd of the anal canal
Discuss the function of large bowel?
The primary function of the large bowel is the reabsorption of water and inorganic salts. It also secretes mucus, which acts as a lubricant during the transport of the intestinal contents.
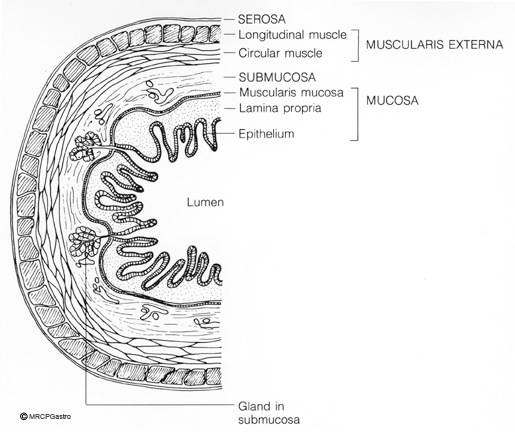
Discuss the histology of large bowel?
Mucosa- is flat with no villi or plica circularis as in small bowel
Surface epithelium- is composed of tall columnar epithelium and goblet cells. Paneth cells (secreting antibacterial substances like lysozyme) are usually present in the caecum & proximal colon (usually confined to the crypt bases). Crypts of Lieberkuhn are straight, narrow and mostly unbranched, separated by a thin rim of lamina propria
Lamina propria- There is only little lamina propria squeezed between glands. It is composed of loose, areolar connective tissue which appears highly cellular due to the presence of chronic inflammatory cells in the superficial part of the lamina propria.
Inflammatory cells in the deeper part and separation of crypt bases from muscularis mucosae by plasma cells and lymphocytes is indicative of IBD.
Muscularis mucosae- 2 layers inner circular and outer longitudinal
Submucosa
Loose connective tissue, also contains Meissner’s plexus of autonomic nerve fibres
Muscle layer- inner circular and outer longitudinal layer of muscle. The outer longitudinal muscle layer forms three flattened strands, the taenia coli. Only a thin layer of longitudinal muscle surrounds the inner circular muscle layer between the taenia coli. The taenia converges at the root of the appendix and the rectum.
Serosa or adventitia- forms small pouches (appendices epiploicae) filled with fatty tissue along the large intestine.
Source: National Cancer Institute






